As cases of COVID-19 continue to mount across the country, evidence shows that the ongoing pandemic disproportionately impacts Black Americans.
According to the latest CDC COVID-19 surveillance summary (ending May 30th), the overall cumulative COVID-19-associated hospitalization rate in the United States among non-Hispanic Black people is 4.5 times that of non-Hispanic White people. Amidst this backdrop, the recent deaths of Breonna Taylor and George Floyd due to police brutality as well as the subsequent protests on social injustice have brought the discussion of health inequity into sharper relief. For instance, earlier this week the American Medical Association pledged action to confront systemic racism and police brutality in a statement that called racism an urgent public health crisis.
In 1985, the Heckler Report, the first federally convened research study on health inequity in the United States, identified higher illness and death rates among minorities (NIH). More recently, the 2017 Robert Wood Johnson Foundation commissioned Communities in Action: Pathways to Health Equity report (a year-long analysis by a 19-member committee of experts in national public health, healthcare, civil rights, social science, education, research, and business), the results of which found that poverty, structural racism, and discrimination are the primary drivers of health inequity. While these drivers go well beyond healthcare, the practice of medicine and administration of healthcare can and should play an active role in addressing health inequity.
How are physicians’ practices addressing inequities?
Examining the perceptions of individual physicians across specialties and practice-settings can illustrate the extent to which practices are acting to address health inequity.
Across specialties, 74% of physicians are highly concerned about health inequity in the United States (ZoomRx study, fielded 6/8-6/11).
However, this level of concern is not always matched by consistent levels of action taken. Concerned physicians are largely split on whether or not they agree their practices are implementing select recommendations from The Institute for Healthcare Improvement’s 2016 whitepaper, Achieving Health Equity: A Guide for Health Care Organizations (IHI).
Physicians’ recommendations on how biopharma can support health equity
Physicians also emphasized a need for biopharma companies to support health equity through a variety of means. They most commonly cited the need for greater patient financial support for vulnerable populations, particularly Medicare & Medicaid patients given their exclusion from copay assistance.
“They can offer products and resources for patients that have fewer resources. Many financial assistance programs disqualify those on federal support and so many medications, including newer treatments, are simply not affordable.”
“Copay assistance programs that those on Medicaid and Medicare qualify for.”
“Perhaps a program that actively identifies patients in predominantly underserved areas that are using their medications and implements procedures to help with access, compliance, and/or affordability.”
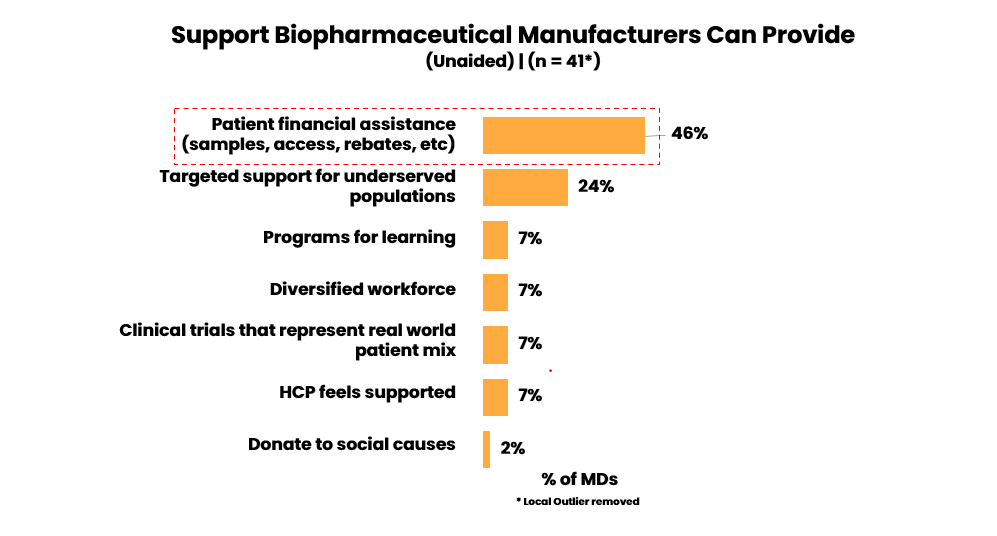
In addition to these calls for greater patient support, some physicians have also called on biopharma manufacturers to examine biases, diversify their workforce, provide equal opportunities, and select partners that share a commitment to health equity. Physicians also saw a need for patient literature that is sensitive to health literacy as well as native language and culture. Lastly, physicians also made note of the role of clinical trials, calling for trial designs that reflect more diverse patient populations and are adequately powered to provide race and ethnicity data cuts.
“Greater conscientiousness regarding their own biases, everything from researching medications in drug trials down to advertisements”
Nevertheless, while physicians clearly outline pathways for greater patient support, they also express low levels of agreement that these pathways currently exist.
Additional ways to advocate for health equity
Even with biopharma manufacturers offering representative support, patient assistance funds, copay programs, in-language patient materials, and other useful services, there are significant unmet needs expressed by physicians. Many in the industry are exploring additional pathways to meet these needs.
In 2019 PhRMA established the Health Equity Roundtable to improve health outcomes by addressing inequalities in care, and last week awarded $25,000 grants to the following:
- AltaMed Blood Pressure Program, which aims to address underlying hypertension, a health disparity impacted by COVID-19, among minority populations in southeast Los Angeles. The partnership facilitates at-home blood pressure monitoring; offers educational materials; and provides support for medication adherence.
- National Spanish Language COVID-19 Prevention Messaging, which aims to address health information gaps in underlying health conditions and their impact on COVID-19 among Hispanic populations by providing essential up-to-date, first-hand COVID-19 information in Spanish.
- Comprehensive Medication Management Program for Vulnerable Populations, which aims to reduce risk for its patients – who are high-risk, low-income, and disproportionately African American – through chronic disease management and medication adherence improvement.
- Implicit Bias Training for Professionals and Community Leaders, which aims to address implicit bias, a key contributor to racial health disparities, and support health providers and community organizations in more equitable service delivery and the reduction of health disparities by race.
The initiatives above demonstrate the variety of diverse and multi-disciplinary efforts that can be undertaken to address this urgent issue. In addition to providing direct patient support, biopharma companies have a variety of strengths and expertise that can and should be utilized towards advancing health equity.
Join ZoomRx and earn while sharing your perspective on key events and the latest therapies.

